Guide to Post-Concussion Syndrome: Tips for Coping with Post-Concussion Syndrome
Guide to Post-Concussion Syndrome: Tips for Coping with Post-Concussion Syndrome

Post-concussion syndrome is a condition that often goes underestimated and misunderstood. It is a formidable challenge for those who have experienced a mild traumatic brain injury, such as a concussion. While concussions are often associated with sports-related injuries, they can happen in everyday situations, including car accidents and falls. Some of the symptoms might continue months or years after the initial injury occurred.
Remember, you are not alone on this path. In the U.S. alone, over 1.5 million traumatic brain injuries happen every year. Seek professional concussion support, lean on your loved ones and be gentle with yourself. By using these helpful tips and techniques confidently, you can start working towards feeling better and having a brighter future, even with PCS.
Managing PCS means being patient with yourself and the healing process. This post-concussion syndrome guide will help you understand these symptoms and, more importantly, how to handle them well.
Table of Contents
What Is Post-Concussion Syndrome?
PCS is not a single injury or a separate medical condition. It is a persistence of concussion symptoms weeks, months or even years after the initial head injury. While most people get better from a concussion fairly quickly, people with PCS have a variety of physical, thinking and emotional symptoms that last longer than usual.
Common Symptoms
Some may experience only a few symptoms, while others contend with a broader range. Each person has a different experience. How long symptoms stick around in PCS also varies between individuals, ranging from a few weeks to several months or years. This is unlike the short-lived symptoms of a regular concussion.
Managing these symptoms is a central part of coping with post-concussion syndrome. Here are some of the most frequently reported symptoms:
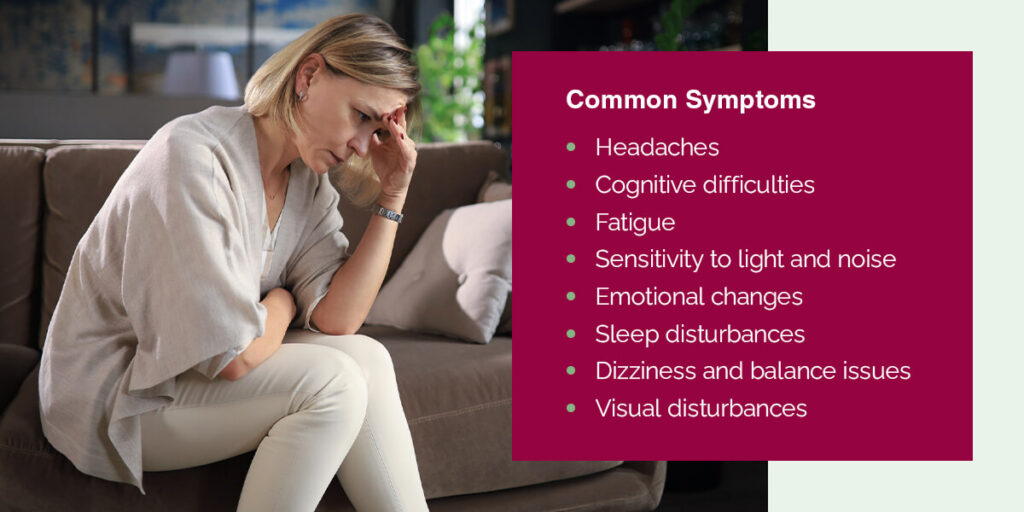
- Headaches: Persistent and often severe headaches are a hallmark of PCS. These headaches can range from tension-type headaches to migraines and may be triggered or exacerbated by activities that require mental concentration.
- Cognitive difficulties: Many individuals with post-concussion syndrome experience difficulties with thinking, memory and concentration. They may struggle to focus, find it challenging to remember recent events or tasks and may experience a mental “fogginess” that makes everyday tasks more challenging.
- Fatigue: Unexplained and overwhelming fatigue is a common complaint among PCS patients. Even simple, routine activities can lead to extreme exhaustion, necessitating more rest and downtime.
- Sensitivity to light and noise: Individuals with PCS often report increased sensitivity to light (photophobia) and noise (phonophobia). Bright lights and loud noises can become intolerable and exacerbate symptoms like headaches.
- Emotional changes: Mood swings, irritability and increased anxiety or depression are common in post-concussion syndrome.
- Sleep disturbances: Many PCS sufferers experience insomnia or disrupted sleep, making it difficult to get the restorative sleep needed for healing.
- Dizziness and balance issues: Vestibular symptoms, such as dizziness and problems with balance, are prevalent in PCS.
- Visual disturbances: Changes in vision, including blurred vision or difficulty focusing, are also reported.
The Persistence of Symptoms
What distinguishes post-concussion syndrome from a typical concussion is the duration of symptoms. This persistence often leads to frustration and confusion for individuals experiencing PCS and their health care providers.
Causes of Post-Concussion Syndrome
The exact mechanisms behind why some individuals develop PCS while others do not remain a subject of ongoing research. Experts believe it may be a mix of things, like how bad the first injury was and your personal tendencies and feelings. Neck injuries are also a potential contributor to concussion symptoms.
A leading chiropractic researcher, Dr. Scott Rosa, has published extensively on “Craniocervical Junction Syndrome” which contributes to brain injury symptoms. Dr. Rosa has treated many high profile patients, including Jim McMahon, former Chicago Bills quarterback. I his article, “Craniocervical Junction Syndrome: Anatomy of the Craniocervical and Atlantoaxial Junctions and the Effect of Misalignment on Cerebrospinal Fluid Flow”, Dr. Rosa outlines the significant impact a head injury can have on the upper neck and the interuption of the proper flow of cerebral spinal fluid (CSF). The disruprion of CSF flow can lead to neurological symptoms and over the long term may cause damage to the brain if the mechanics of the upper neck are not corrected.
Seeking Help and Diagnosis
If you or a loved one suspect PCS, it is crucial to seek medical attention. An authoritative diagnosis from a health care professional, typically a neurologist or neuropsychologist, is a good place to start in seeking help. Once you know the extent of your condition, you can begin a path to symptom management.
6 Tips for Coping with Post-Concussion Syndrome
Navigating PCS is best done with a team of professionals by your side. Advice from medical experts, neurologists and neuropsychologists is crucial in tailoring a treatment plan that suits your specific needs. These experts can help you understand your symptoms, set realistic goals and track your progress. Here are some tips for post-concussion syndrome:
- Implement cognitive rest: Rest is a cornerstone of PCS recovery. Prioritize restorative sleep as often as possible. Take it easy on your brain by avoiding things like excessive screen time or heavy reading, especially when your eyes are tired or you’re experiencing other symptoms.
- Establish a support system: Lean on your loved ones for emotional support. Consider joining support groups or online communities where you can connect with others with similar experiences.
- Manage stress and anxiety: PCS often brings heightened stress and anxiety levels. Learning stress-reduction techniques, such as meditation or deep breathing exercises, can help you regain control over your emotional well-being.
- Keep a symptom journal: Authoritative management of PCS requires a systematic approach. Keeping a detailed symptom journal can assist you and your health care team in tracking patterns and identifying potential triggers. This can lead to more effective treatment adjustments and give you a better idea of what to expect from PCS moving forward.
- Explore rehabilitation therapies: Certain therapies, like vestibular and cognitive rehabilitation, have shown promise in managing PCS symptoms.
- Upper Cervical Chiropractic Care: Another treatment to consider is gentle spinal correction by chiropractic experts. Consult with your health care team to determine whether these therapies suit your situation.
- Healthy diet and hydration: Eating a balanced diet rich in nutrients can support your brain’s healing process. Focus on foods with antioxidants such as omega-3 fatty acids, fruits and vegetables. Stay well-hydrated, as dehydration can exacerbate symptoms. Consult with a professional nutritionist or dietitian to help tailor a diet to your needs.
Contact UCC of Monmouth for Support
We’ve explored the nuances of PCS, from its definition and common symptoms to the importance of seeking professional diagnosis and support. Now, let’s introduce a unique perspective that can complement your approach to managing post-concussion syndrome.
Upper Cervical Chiropractic of Monmouth, LLC, offers an innovative and gentle approach to healing that can be particularly valuable to those dealing with PCS. Our expertise lies in addressing the delicate balance within the spine and nervous system, starting with the first vertebra in the neck, the C-1 vertebra, also known as the Atlas.
For those with PCS, this gentle correction offered by Upper Cervical Chiropractic of Monmouth, LLC, can be a valuable adjunct to their treatment plan. By addressing the root causes of nerve pressure and spinal misalignment, this approach aims to enhance the overall healing process.
Take another step toward regaining your well-being by integrating the expertise of professionals like Upper Cervical Chiropractic of Monmouth, LLC.

Dr. Arbeitman
Dr. Arbeitman, a trailblazing figure in Upper Cervical Chiropractic, established Upper Cervical Chiropractic of Monmouth, LLC in 2005. Dedicated to promoting holistic wellness, he has empowered countless individuals to embrace Upper Cervical Chiropractic care as an integral part of their health journey. Graduating Magna Cum Laude from Logan College of Chiropractic and holding a Bachelor of Science in Kinesiological Sciences from the University of Maryland at College Park, Dr. Arbeitman is a licensed practitioner in New Jersey who has met the rigorous standards set by the National Board of Chiropractic Examiners. Beyond his extensive educational achievements, he has earned multiple scholarships and accolades for his academic prowess and exemplary clinical performance. Dr. Arbeitman's holistic approach encompasses spinal and nervous system care, lifestyle guidance, fitness evaluation, and nutritional expertise, all founded on the belief that the doctor-patient relationship is paramount to the healing process.